
Total Knee
Replacement (TKR)
Total Knee
Replacement (TKR)
Knee replacement is the resurfacing of the worn out surfaces of the knee and replacing the lost cartilage and diseased bone with metal and plastic. The main reason for replacing any JOINC is to Stop the exposed bone ends rubbing together causing pain. Replacing the painful arthritic joint with an artificial joint prosthesis gives the joint new surfaces that move smoothly and without causing pain.
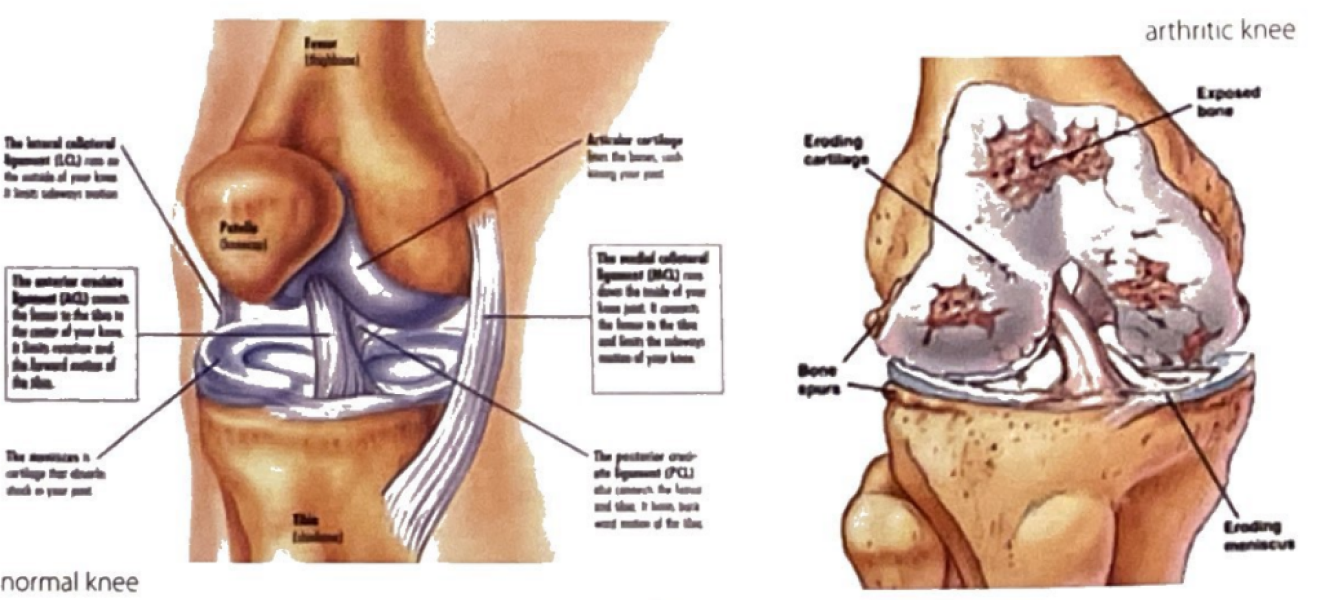
Knees wear out for a variety of reasons, including inflammation from arthritis, injury, or simply wear and tear Sometimes only part of the knee 1s damage and an uni-condylar knee prosthesis 15 used partial knee replacement It only replaces the worn surfaces on one side of the knee joint it is less extensive which mean recovery is faster. The goal is to help you return to normal activities without pain. Surgery involves removing the damaged cartilage and bone and positioning the new metal and plastic joint surfaces to restore the alignment and function of the knee
Advantages Include:
- Relief from knee pain
- Increased mobility
- Improved function
- Less muscle weakness
- Reduce dependencies on medication
- Rapid recovery
- Less risk of dislocations
- Early discharge home
PROCEDURE DETAIL
In-Depth Treatment Insights
-
Minimally Invasive knee replacement
Minimally Invasive knee replacement involves the use of smaller incision than tne one used in traditional knee replacement. In the traditional method, the incision averages 8 to 10 inches in length. In minimally invasive knee surgery, the incision is only 4 to 6 inches long, because there 15 less damage to the tissue around the knee, patients who undergo this procedure may expect a shorter hospital stay, a shorter recovery, and a better looking scar.
More than 90% o f individuals expenence a dramatic reduction in pain and significant improvement in the ability t o perform common activities of daily living following hip replacement surgery
However you may be advised t o avoid some types o f activity including jogging and high impact sports for the rest of your life Your surgeon will advise you further on this.
-
Risk or Side Effects
- Reaction to the anaesthetic drugs used
- Bleeding or deep bruising
- Wound Infection
- Nerve injury
- Residual pain and swelling
- Blood clots - could form in the legs called Deep Vein Thrombosis (DVT). Rarely one of these clots may travel to your jungs. To help prevent blood clot
- You will be on blood thinning medications
- You will have inflatable leg coverings (foot pumps)
- You will be asked t o wear special support stockings {TEDs)
- You will be encouraged to do ankle pump exercises
- You will be mobilized early out of bed
-
Preparing for the Surgery
Surgeon will arrange MRSA screening prior your admission. Please consult your dentist prior to your surgery to check for any signs of infection.
Please bring in the following items:
1. All current medications in their original boxes if possible. If you are taking blood thinners (e.g. Warfarin,Plavix or Asprin etc), please inform your consultant at least one week before surgery as these may need t o be stopped a few days before surgery.
2. X-ray films and discs.
3. Day clothes - loose, comfortable clothing (shorts, tracksuit or skirts are ideal).
4. Footwear - comfortable lace up or slip-on
shoes with low heels, flat if poss.ble.Trainers of runners are ideal but not nesessary. We do not recommend old slipper, or backless
shoes. Do not wear tight hitting footwear as the operated leg/foot may excet ence some temporary swelling after surgery
5. Night clothes - pyjamas, nightdiesses, dressing gown, slippers with backs
-
Day of Surgery
1. You will be admitted day o f surgery, time to be confirmed.
2. Shower should be taken to ensure your skin is adequately prepared for the surgery, the night before and the morning of the surgery (prior to admission).
3. You will also be required to change into a hospital gown
4. Ananaesthetist will see you prior to anaesthetic to discuss the options available for anaesthetic and pain relief
5. Aphysiotherapist will review your exercises and mobilize you.
6. Anurse will apply a calf pump machine which helps prevent clot formation in your legs, so that you are a aware what it will feel like after surgery.
-
After the Surgery
1. When you wake u p from surgery you
will be in the recovery room. You will be given oxygen through a facemask and an intravenous drip (which gives you fluid directly Into a vein). You will be monitored by a nurse until you are ready to be transferred back to the ward.
2. On return to the ward a nurse will closely monitor your vital signs.
3. As you recover fully from the anaesthetic, you will be assisted by the physiotherapist and Nurse to sit up and mobilize out o f bed.
4. You may have a urinary cathedral in place after the surgery. This will drain urine automatically from the bladder it is usually removed after surgery.
5. You may also have drain from your wound which will drain excess blood from the wound it is generally taken out the next morning also.
6. It is essential you perform deep breathing and foot pump exercises as explained to you by physiotherapist.
7. Your exercise and physiotherapy program will be guided by the physiotherapist and will gradually increase over the next few days until you are discharged.
8. Your wound dressing will be checked regularly by the nurse to ensure that there is no sign of infection or bleeding This dressing
will be changed as needed
9. The estimated length o f hospital stay is 3-4 days after surgery but the exact time will depend on your progress after surgery.
-
Discharge Instruction
Most people g o home using one or two crutches to support their new knee. You should be able to walk without a limp before you discard your crutches.
You can gradually increase your level of activity and should continue your exercise program until you are reviewed by your surgeon (usually 6-8 weeks). You should continue to improve for several months.
-
Diet, Medication, Activity Guidelines, Dressing, Follow Up
Diet:
- Resume your regular diet as tolerated.
- It is important to eat plenty of fibre (to prevent constipation), protein and vitamin C (to promote wound healing).
- Drink ptenty of fluids throughout the day(recommended 2-3 liters/ day).
Medication:
- Resume your pre-surgery medications, Blood thinners may be delayed by surgeon.
- You will be given a prescription by the surgeon for painkillers, anti inflammatories and a blood thinning medication.
Activity Guidelines:
1. HOBBIES - acceptable activities include:
- Golfing
- Gardening
- Dancing
- Walking
- Swimming - once sutures have been removed and the wound is healed (avoid breast stroke)
- Cycling (on level surface) at 6-8 weeks and at your surgeon's discretion.
2. Avoid activities that put stress on the knee:
- Tennis, squash
- Football, baseball
- Jumping
- Weight lifting more than 40lbs
Dressing:
- Do not get the wound or dressing wet. It is advised to get assistance when showering for the first few days.
- Observe the knee site for any redness/ heat/yellow discharge.
- Your wound will be closed with stitches, clips or glue. You will be advised of this before you are discharged.
- If you have stitches or clips, they will be removed generally 10-14 days after the surgery.
- Contact your surgeon or the hospital if you have any concerns.
Follow Up:
- You will be given date to return t o the hospital for removal o f stitches or clips or advised to go to your GP.
- You will have a follow up appointment after 6-8 weeks approximately. This will be arranged by your surgeon secretary.
- You will be contacted by a nurse t o enquire about your progress within 2-3 months following your discharge.
-
General advice
Progression is largely dependent on you. You must exercise regularly to regain movement, strength and independence. Periods o f rest in between are equally important. Do not sit still for too long. Get up and walk and exercise regularly. Little and often is the key. By approximately 3 months post-op you will be largely back to your normal activities, although improvement continues for up to a year.
-
Points to remember
- Avoid excessively twisting your knee when turning: always lift up your feet
- Do not sit or lie with a pillow under your knee - this may cause a permanently bent knee
- Avoid kneeling for 1 year
- Stand with your weight evenly distributed through each foot
- Do not drive until your strength and speed of movement are up to coping with an emergency stop.This Is also at the discretion of your consultant. You should always speak with your insurance company before coming into hospital as your insurance policy may be affected
- Use Ice Packs and Elevation Wedge regularly during the day it hetps control swelling and relieves pain.
Once you are home you must continue with all of your exercises.
Do not hesitate to ask your Physiotherapist any questions. We would like you to be sure what to do once you go home.
Want to know further information?
A further detailed information sheets/booklet will be given by Mr. Mahalingam to his patients undergoing specific surgical procedures outlining pre-operative preparation/instructions and all
ENQUIRY
Inquire with
Confidence
Contact Us
We will get back to you as soon as possible.
Please try again later.
100+
Bikini Hip Replacement Surgery
120+
Anterior Hip Replacement Surgery
200+
Knee Replacement Surgery
PROCEDURE DETAILS
In-Depth Treatment Insights
Minimally invasive knee replacement
Minimally Invasive knee replacement involves the use of smaller incision than tne one used in traditional knee replacement. In the traditional method, the incision averages 8 to 10 inches in length. In minimally invasive knee surgery, the incision is only 4 to 6 inches long, because there 15 less damage to the tissue around the knee, patients who undergo this procedure may expect a shorter hospital stay, a shorter recovery, and a better looking scar.
More than 90% o f individuals expenence a dramatic reduction in pain and significant improvement in the ability t o perform common activities of daily living following hip replacement surgery
However you may be advised t o avoid some types o f activity including jogging and high impact sports for the rest of your life Your surgeon will advise you further on this.
Who is Suitable?
- Reaction to the anaesthetic drugs used
- Bleeding or deep bruising
- Wound Infection
- Nerve injury
- Residual pain and swelling
- Blood clots - could form in the legs called Deep Vein Thrombos!s (DVT). Rarely one of these clots may travel to your jungs. To help prevent blood clot
- You will be on blood thinning medications
- You will have inflatable leg coverings (foot pumps)
- You will be asked t o wear special support stockings {TEDs)
- You will be encouraged to do ankle pump exercises
- You will be mobilized early out of bed
Preparing for the surgery
Surgeon will arrange MRSA screening prior your admission. Please consult your dentist prior to your surgery to check for any signs of infection.
Please bring in the following items:
1. All current medications in their original boxes if possible. If you are taking blood thinners (e.g. Warfarin,Plavix or Asprin etc), please inform your consultant at least one week before surgery as these may need t o be stopped a few days before surgery.
2. X-ray films and discs.
3. Day clothes - loose, comfortable clothing (shorts, tracksuit or skirts are ideal).
4. Footwear - comfortable lace up or slip-on
shoes with low heels, flat if poss.ble.Trainers of runners are ideal but not nesessary. We do not recommend old slipper, or backless
shoes. Do not wear tight hitting footwear as the operated leg/foot may excet ence some temporary swelling after surgery
5. Night clothes - pyjamas, nightdiesses, dressing gown, slippers with backs
Day of surgery
1. You will be admitted day o f surgery, time to be confirmed.
2. Shower should be taken to ensure your skin is adequately prepared for the surgery, the night before and the morning of the surgery (prior to admission).
3. You will also be required to change into a hospital gown
4. Ananaesthetist will see you prior to anaesthetic to discuss the options available for anaesthetic and pain relief
5. Aphysiotherapist will review your exercises and mobilize you.
6. Anurse will apply a calf pump machine which helps prevent clot formation in your legs, so that you are a aware what it will feel like after surgery.
After the surgery
1. When you wake u p from surgery you
will be in the recovery room. You will be given oxygen through a facemask and an intravenous drip (which gives you fluid directly Into a vein). You will be monitored by a nurse until you are ready to be transferred back to the ward.
2. On return to the ward a nurse will closely monitor your vital signs.
3. As you recover fully from the anaesthetic, you will be assisted by the physiotherapist and Nurse to sit up and mobilize out o f bed.
4. You may have a urinary cathedral in place after the surgery. This will drain urine automatically from the bladder it is usually removed after surgery.
5. You may also have drain from your wound which will drain excess blood from the wound it is generally taken out the next morning also.
6. It is essential you perform deep breathing and foot pump exercises as explained to you by physiotherapist.
7. Your exercise and physiotherapy program will be guided by the physiotherapist and will gradually increase over the next few days until you are discharged.
8. Your wound dressing will be checked regularly by the nurse to ensure that there is no sign of infection or bleeding This dressing
will be changed as needed
9. The estimated length o f hospital stay is 3-4 days after surgery but the exact time will depend on your progress after surgery.
Discharge Instruction
Most people g o home using one or two crutches to support their new knee. You should be able to walk without a limp before you discard your crutches.
You can gradually increase your level of activity and should continue your exercise program until you are reviewed by your surgeon (usually 6-8 weeks). You should continue to improve for several months.
Diet, Medication,Activity Guidelines, Dressing & Follow Up
Diet:
- Resume your regular diet as tolerated.
- It is important to eat plenty of fibre (to prevent constipation), protein and vitamin C (to promote wound healing).
- Drink ptenty of fluids throughout the day(recommended 2-3 liters/ day).
Medication:
- Resume your pre-surgery medications, Blood thinners may be delayed by surgeon.
- You will be given a prescription by the surgeon for painkillers, anti inflammatories and a blood thinning medication.
Activity Guidelines:
1. HOBBIES - acceptable activities include:
- Golfing
- Gardening
- Dancing
- Walking
- Swimming - once sutures have been removed and the wound is healed (avoid breast stroke)
- Cycling (on level surface) at 6-8 weeks and at your surgeon's discretion.
2. Avoid activities that put stress on the knee:
- Tennis, squash
- Football, baseball
- Jumping
- Weight lifting more than 40lbs
Dressing:
- Do not get the wound or dressing wet. It is advised to get assistance when showering for the first few days.
- Observe the knee site for any redness/ heat/yellow discharge.
- Your wound will be closed with stitches, clips or glue. You will be advised of this before you are discharged.
- If you have stitches or clips, they will be removed generally 10-14 days after the surgery.
- Contact your surgeon or the hospital if you have any concerns.
Follow Up:
- You will be given date to return t o the hospital for removal o f stitches or clips or advised to go to your GP.
- You will have a follow up appointment after 6-8 weeks approximately. This will be arranged by your surgeon secretary.
- You will be contacted by a nurse t o enquire about your progress within 2-3 months following your discharge.
General advise
Progression is largely dependent on you. You must exercise regularly to regain movement, strength and independence. Periods o f rest in between are equally important. Do not sit still for too long. Get up and walk and exercise regularly. Little and often is the key. By approximately 3 months post-op you will be largely back to your normal activities, although improvement continues for up to a year.
Points to remember
- Avoid excessively twisting your knee when turning: always lift up your feet
- Do not sit or lie with a pillow under your knee - this may cause a permanently bent knee
- Avoid kneeling for 1 year
- Stand with your weight evenly distributed through each foot
- Do not drive until your strength and speed of movement are up to coping with an emergency stop.This Is also at the discretion of your consultant. You should always speak with your insurance company before coming into hospital as your insurance policy may be affected
- Use Ice Packs and Elevation Wedge regularly during the day it hetps control swelling and relieves pain.
Once you are home you must continue with all of your exercises.
Do not hesitate to ask your Physiotherapist any questions. We would like you to be sure what to do once you go home.
Want to know further information?
A further detailed information sheets/booklet will be given by Mr. Mahalingam to his patients undergoing specific surgical procedures outlining pre-operative preparation/instructions and all
ENQUIRY
Inquire with Confidence
Contact Us
We will get back to you as soon as possible.
Please try again later.
100+
Bikini Hip Replacement Surgery
120+
Anterior Hip Replacement Surgery
200+
Knee Replacement Surgery
ENQUIRY
Inquire with Confidence
Contact Us
We will get back to you as soon as possible.
Please try again later.
